A parent's guide to autism evaluations in Western Australia
There is a HUGE amount of confusion around for families trying to work out what evidence they need to provide of their child’s autism diagnosis. Many families are sitting on waitlists to see a paediatrician not knowing they may be able to access support from their school and the NDIS without it.
Private assessments are expensive – families are forking out about $3,000 for assessments and reports per child. Consider the impact of that when a family has multiple children requiring assessment.
Families are “triaging” their child who is most in need of support as who can afford the cost of one, let alone two or three assessments? Or face a 3.5 year wait via the Child Development Services for an autism assessment with little to no support in the interim.
One of the challenges families face is that they are dealing with up to four different government departments as they seek to secure help for their child. Two Federal: Medicare and NDIS and two State-based: Health and Education.
I have tried to collate the information all in one place so that you can make the best decision on how to support your child.
Table of Contents
Medicare
In March 2023 a Medicare rebate was introduced for people aged 0-25 years seeking diagnosis of complex neurodevelopmental disorders and disabilities, including autism.
To receive the rebate you need a GP to refer you to a paediatrician or psychiatrist. The paediatrician or psychiatrist then refers you onto allied health practitioners for assessment.
Which is great in theory, but just means more people are trying to get in to see a paediatrician and psychiatrist for an initial referral. And we all know that’s near on impossible.
Given that both NDIS and Department of Education now do not require a paediatrician or psychiatrist to sign off on an autism diagnosis, many families are going without the Medicare rebate so that they can speed up the process.
Read more here: Services Australia: Manage complex neurodevelopmental disorders and eligible disabilities
If your child is under the age of 6
For children under the age of 6 years, a formal autism diagnosis is NOT required to apply for access to the NDIS. If you are concerned that your child has delays in two or more areas should contact Wanslea who can help you determine if your child might be eligible for NDIS access.
If your child has turned 7
If your child has turned 7 and you are accessing the Early Childhood Approach for developmental delay please be prepared that you will be contacted by the NDIA for a reassessment of eligibility.
The NDIS is currently exiting a record number of children off the program who have been accessing support for developmental delay or disabilities that the NDIA do not recognise as permanent impairments. (Even though in many cases they are.)
For more information read the blog I have written: A Parent’s Guide to NDIS Eligibility Reassessments.
National Disability Insurance Scheme (NDIS)
NDIA Evidence of Disability: Autism
The NDIA requires a comprehensive diagnostic assessment to be completed by a specialist multi-disciplinary team, paediatrician, psychiatrist or clinical psychologist experienced in the assessment of Pervasive Developmental Disorders and assessed using the current Diagnostic and Statistical Manual of Mental Disorders (DSM-V) diagnostic criteria.
Does the NDIS accept an assessment by a psychologist?
The NDIS access team has confirmed that a Lead Practitioner Diagnostic Evaluation Level 2 or Level 3 autism diagnosis by a:
- clinical psychologist,
- clinical neuropsychologist or
- educational and developmental psychologist
experienced in autism assessments is sufficient evidence of a “List A” condition.
List A conditions are conditions that are likely to meet the disability requirements for access to the NDIS.
The NDIS will not accept a Lead Practitioner Diagnostic Evaluation completed by a:
- registered psychologist,
- provisional psychologist,
- clinical psychology registrar, neuropsychology registrar,
- or educational and developmental psychology registrar
These practitioners may form part of a Consensus Team Diagnostic Evaluation.
Does the NDIS require an autism assessment to be signed off by a paediatrician?
The NDIS only requires consensus by a paediatrician or psychiatrist of an autism diagnosis IF the diagnostic evaluation prepared by the psychologist states that an opinion or conferral of the diagnosis is required.
Then, the NDIS will expect that report at some point in the future to confirm diagnosis.
This is a different requirement from access to the Individual Disability Allocation through the Department of Education.
Future applications
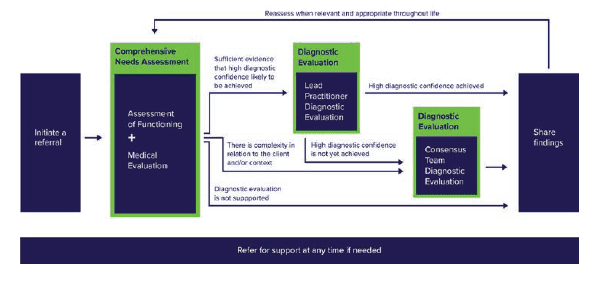
Comprehensive Needs Assessment and Diagnostic Evaluation
The NDIA has flagged moves to align with recommendations of the Autism CRC’s guidelines for the assessment and diagnosis of autism in Australia.
This includes that: “future applications may benefit from evidence such as details of a Comprehensive Needs Assessment (comprising of an assessment of functioning and medical evaluation) and Diagnostic Evaluation (single clinician diagnostic evaluation and, if required, consensus team diagnostic evaluation.)”.
Lead Practitioner Diagnostic Evaluation
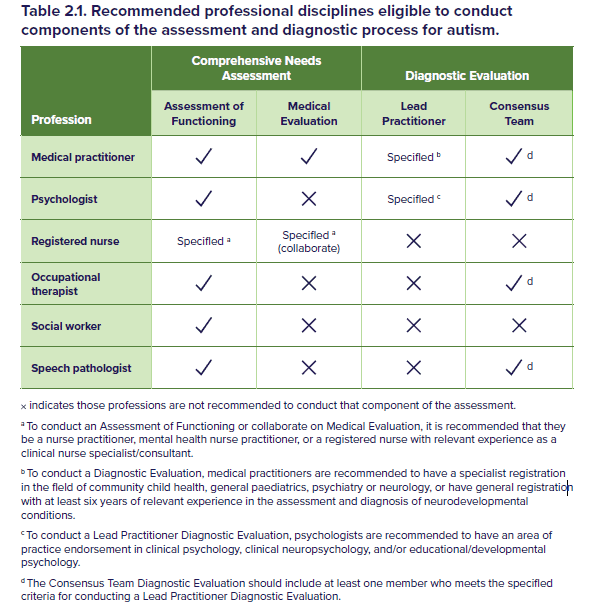
The Autism CRC’s National Guideline for the assessment and diagnosis of autism states that a Lead Practitioner Diagnostic Evaluation should be conducted by one practitioner meeting at least one of the following:
- Medical practitioner who holds specialist registration with the Medical Board of Australia in the field of community child health, general paediatric, psychiatry or neurology
- Medical practitioner who holds general or specialist registration with the Medical Board of Australia and has at least six years of relevant experience, training or supervision in the assessment of neurodevelopmental and behavioural disorders
- Psychologist who holds general registration with the Psychology Board of Australia and an area of practice endorsement in clincial psychology, clinical neuropsychology and/or educational/developmental psychology with the Psychology Board of Australia.
Specialist Multidisciplinary Team
As of yet, the NDIA have not been able to confirm for me which combination of specialists is required to form a “specialist multidisciplinary team”.
The Autism CRC recommends that a Consensus Team Diagnostic Evaluation should include at least one additional practitioner who meets at least one of the following eligibility critieria:
- Medical practitioner who holds specialist registration with the Medical Board of Australia in the field of community child health, general paediatrics, psychiatry or neurology.
- Medical practitioner who holds general or specialist registration with the Medical Board of Australia and has at least six years of relevant experience, training or supervision in the assessment of neurodevelopmental disorders.
- Occupational therapist who holds registration with the Occupational Therapy Board of Australia.
- Psychologist who holds general registration, with or without an area of practice endorsement in clinical psychology, clinical neuropsychology, and/or educational/developmental psychology with the Psychology Board of Australia.
- Speech pathologist who is eligible to be a certified practicing member of Speech Pathology Australia.
(Updated 25/2/2025)
Co-occurring conditions & medication considerations
Medication Prescription
Autism frequently co-occurs with ADHD, anxiety and depression. Psychologists can diagnose these conditions but they cannot prescribe medications.
GPs can prescribe anti-depressants such as Fluoxetine however many are reluctant to do so for kids.
Stimulant medications such as dexamphetamine can only be initiated by a paediatrician, psychiatrist or neurologist. Once the medication type and dose is stabilised then you can ask your paediatrician, psychiatrist or neurologist to request authorisation for your GP to become a co-prescriber.
Updated 21 November 2024.
Western Australian Department of Education
The information provided below was provided by the Department of Education in their submission to the Parliamentary Inquiry into autism in schools (2023) and is supplemented by updated advice from the Disability and Inclusion team.
I have included a few clarifications in [square brackets] to make the information clearer.
Eligible practitioners
Students can be assessed for autism using a single practitioner pathway or a consensus team pathway.
The choice of practitioner and the number of practitioners involved in the assessment of functioning is determined by the assessment team.
This is applied to students of all ages.
Single Clinician Pathway
If a single practitioner pathway is taken, the ASD assessment is conducted by either a:
• medical practitioner with specialist registration in community child health, general paediatrics, psychiatry or neurology, or who has a general registration with at least six years of relevant experience in assessing neurodevelopmental disorders
[OR]
• psychologist with practice endorsement in clinical psychology, educational or developmental psychology, or neuropsychology.
[AND]
The diagnosis must be verified by an:
- eligible second practitioner with skills and expertise in the assessment and diagnosis of autism
- from a different discipline or specialty.
Consensus Team Pathway
If a consensus team pathway is taken, the ASD assessment is conducted by either a:
• medical practitioner with specialist registration in community child health, general paediatrics, psychiatry or neurology,
[OR]
- medical practitioner who has a general registration with at least six years of relevant experience in assessing neurodevelopmental disorders
[OR]
• a psychologist with practice endorsement in clinical psychology, educational or developmental psychology, or neuropsychology.
[AND]
At least one additional diagnostician is selected to join the diagnostic team.
The decision is based on their skills and expertise and can be:
• a psychologist with general registration
• a speech pathologist
• an occupational therapist who has experience assessing ASD.
Eligibility requirements for supplementary funding
Schools may apply for an Individual Disability Allocation for students with a disability.
Eligibility for this funding is based on 8 disability categories (ASD, deaf and hard of hearing, global developmental delay, intellectual disability, physical disability, severe medical health condition, severe mental disorder and vision impairment).
Explicit criteria are applied and evidence of eligibility against each criterion is required from relevant medical practitioners or professionals.
Eligibility for an IDA in the ASD category is in accordance with:
• Diagnostic and Statistical Manual of Mental Disorders – 5th edition (DSM-5, American Psychiatric Association, 2014
• National Guideline for the Assessment and Diagnosis of Autism Spectrum Disorder in Australia.
Interim IDA while the student is on a waitlist for assessment
Students are eligible for an interim IDA if they can provide a letter from the assessing practitioners or government agency confirming they:
• have been accepted for an ASD assessment
• are on the waitlist for assessment
• have an ASD assessment scheduled.
A request for consent or a referral is not considered evidence.
An interim IDA is not available if the student has previously not met the ASD criteria and is re-referred for assessment.
Extension of Interim IDA
On 16 April 2024, The Department of Education confirmed the endorsement of an extension to the initial allocation of interim funding for students undertaking an autism assessment from:
- six months to 12 months for private assessments
- 12 months to 18 months for public assessments.
Eligibility documentation requirements for an Individual Disability Allocation for autism
To be eligible, students need a signed letter, or a statement that is embedded within the text of a full report from eligible practitioner/s.
The letter or statement needs to:
• state the diagnosis
• state the current levels of severity (support, substantial support, or very substantial support)
• specify whether the diagnosis is:
− with or without intellectual impairment
− with or without accompanying language impairment
• list the names of the diagnosing practitioners
• state that all practitioners confer and agree with the diagnosis if the assessment was completed by a consensus team.
If the assessment is undertaken by a single practitioner, a statement from a second practitioner is also required to confirm that:
• the practitioners have conferred following the completion of all assessments
• each practitioner agrees with the diagnosis and levels of severity.
Who applies for the IDA?
School staff submit the application on the family’s behalf.
The application is assessed by the Department to make sure it meets the specific eligibility criteria.
Schools are then allocated a funding level that corresponds to the level of support and the teaching and learning adjustments required by the student.
Principals and school staff determine the specific distribution of these resources to meet the needs of individual students, including implementing teaching and learning adjustments and creating responsive staffing profiles and learning support teams that best meet the needs of their students and school context.
Adjustments may include access to appropriate technology or specialised equipment, modifying the curriculum, alternative methods of assessment, access to an education assistant or accessibility enhancements to the school buildings or grounds.
What if I am unhappy with the outcome or support provided by the school?
Contact the school as early as possible if you have concerns. Talking to your child’s teacher, year coordinator, school administration or principal is the best place to start.
Raise the matter with the principal if:
- you were not able to achieve a satisfactory outcome with the teacher or staff member
- the matter is about the conduct of a teacher or staff member
- the matter is about another aspect of school life that is impacting your child’s education.
Contact the school to request an appointment to discuss your concerns.
Raise the matter with the education regional office if:
- you believe that your concern was not satisfactorily resolved or addressed by the school
- the matter is about the conduct of the principal.
If the matter is not about the conduct of the principal or a previous unsatisfactory resolution, the education regional office may refer it back to the school, unless there is a reason preventing the school from managing it.
You can read more about the complaints process here.

Pia



The Ed Psych Clinic 
- Assessment - ADHD
- +10 Assessment - Autism, Assessment - Dyscalculia (Specific Learning Disorder in Mathematics), Assessment - Dysgraphia (Specific Learning Disorder in Writing), Assessment - Dyslexia (Specific Learning Disorder in Reading), Assessment - Giftedness, Assessment - Intellectual Disability, Assessment - Language Development Centre Referrals, Assessment - SCSA, Assessments - Educational and Cognitive, Psychologist
- 24 Richardson Street, West Perth Western Australia 6005, Australia


TLC WA 
- Assessment - Autism
- +10 Assessment - Developmental Language Disorder (DLD), Dietitian, NDIS Services, Occupational Therapist, Parent / Carer Support, Physiotherapist, Psychologist, Psychologist - Clinical, Speech Pathologist, Speech Pathologist - Feeding
- 10 Elcar Lane, Joondalup Western Australia 6027, Australia


FABIC Behaviour Specialist Centre 
- Assessment - ADHD
- +12 Assessment - Autism, Counsellor, Learning Specialist, NDIS Services, NDIS Support Coordination, Occupational Therapist, Play Therapist, Positive Behaviour Support, Psychologist, Speech Pathologist, Speech Pathologist - Feeding, Training Provider
- 6000, Perth, Western Australia, Australia
House of Mind 
- Assessment - ADHD
- +10 Assessment - Autism, Assessment - Dyscalculia (Specific Learning Disorder in Mathematics), Assessment - Dysgraphia (Specific Learning Disorder in Writing), Assessment - Dyslexia (Specific Learning Disorder in Reading), Assessment - Giftedness, Assessment - Intellectual Disability, Assessments - Educational and Cognitive, Parent / Carer Support, Psychologist, Social Worker
- 41 York Street, Subiaco Western Australia 6008, Australia
Mini Minds Child and Adolescent Health 
- Assessment - Autism
- +9 Assessment - Dyscalculia (Specific Learning Disorder in Mathematics), Assessment - Dyslexia (Specific Learning Disorder in Reading), Assessment - Giftedness, Assessment - Intellectual Disability, Assessments - Educational and Cognitive, Occupational Therapist, Play Therapist, Psychologist, Psychologist - Clinical
- 163 Canning Highway, East Fremantle Western Australia 6158, Australia
Bubbles Speech Pathology 
- Assessment - Autism
- +3 Assessment - Developmental Language Disorder (DLD), Assessment - Language Development Centre Referrals, Speech Pathologist
- 1/100 Walters Drive, Osborne Park Western Australia 6017, Australia

